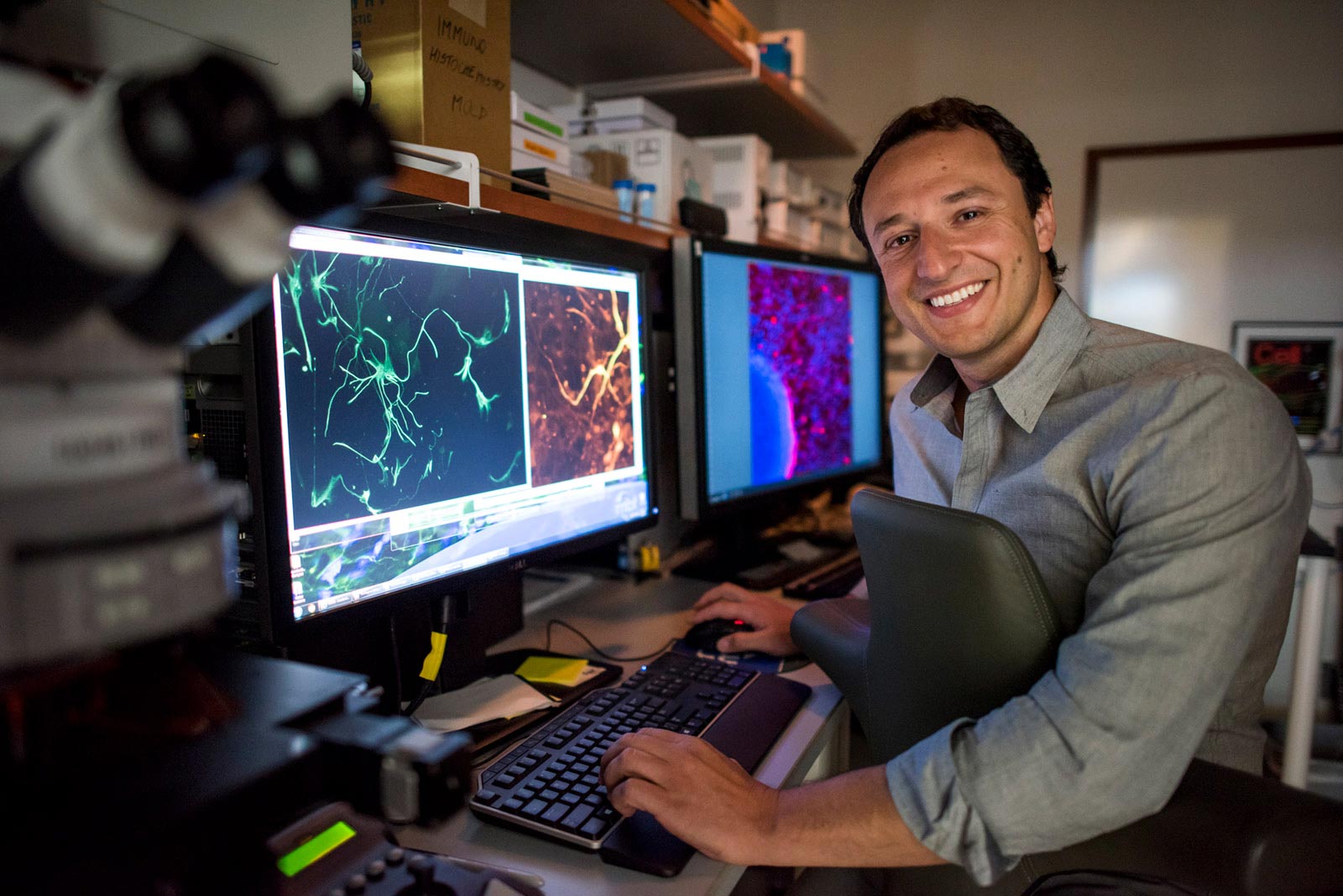
Alysson Muotri, PhD, is Professor and Director of the Stem Cell Program at the UC San Diego School of Medicine and a member of the Sanford Consortium for Regenerative Medicine. Photo credit: UC San Diego Health Sciences
Rett syndrome, a rare form of autism spectrum disorder, affects nearly every part of a child’s life, including movement, speech, and breathing.
Most autism spectrum disorders have a complex, multifactorial genetic component that makes specific treatments difficult to find. Rett syndrome is an exception. Babies born with this form of the disorder have mutations specifically in the MECP2 Gene that causes severe brain development impairment that mainly affects women. However, there is no treatment yet – current therapies aim to relieve symptoms but do not address the root cause.
Researchers at the University of California’s San Diego School of Medicine and the Sanford Consortium for Regenerative Medicine recently used stem cell-derived brain organoids – also known as “mini-brains” – that lack function MECP2 Gene to better study the disease.
In a study published on December 8, 2020 in EMBO Molecular MedicineThe team identified two drug candidates that were affected by the lack of MECP2 Gene. These compounds restored calcium levels, neurotransmitter production, and electrical impulse activity, and returned the organoids in Rett syndrome to near normal levels.
“The gene mutation that causes Rett syndrome was discovered decades ago, but advances in treatment have lagged, at least in part because mouse model studies have not been transferred to humans,” said senior author Alysson R. Muotri, PhD, professor in Pediatrics and Cellular and Molecular Medicine from UC San Diego School of Medicine. “This study was driven by the need for a model that better mimics the human brain.”
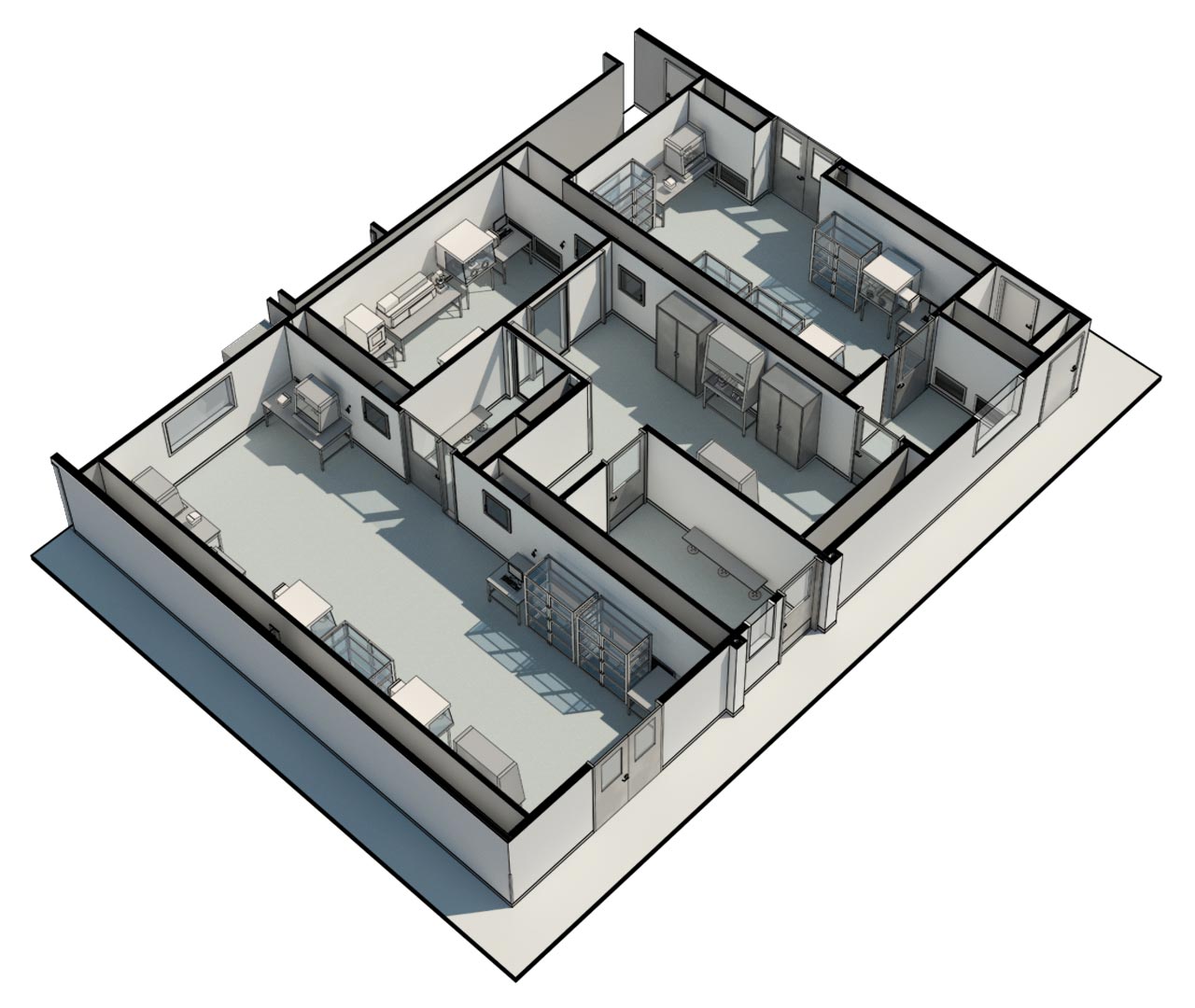
Brain organoids are 3D cell models that represent aspects of the human brain in the laboratory. These organoids help researchers track human development, uncover the molecular events that lead to disease, and test new treatments. At UC San Diego, brain organoids were used to provide the first direct experimental evidence that the Brazilian Zika virus can cause serious birth defects and to reuse existing HIV drugs to treat another rare, inherited neurological disorder. Muotri and his team also sent their brain organoids to the International Space Station to test the effects of microgravity on brain development – and possibly prospects for human life beyond Earth.
They are of course not perfect replicas. Organoids lack connections to other organ systems such as blood vessels. Drugs tested on brain organoids are added directly – they do not have to cross the blood-brain barrier, specialized blood vessels that keep the brain largely free of bacteria, viruses and toxins.
However, researchers find organoids very useful for checking for changes in physical structure or gene expression over time or as a result of a gene mutation, virus, or drug. In addition, Muotri’s team recently optimized the process of organoid assembly in the brain to adapt it to the electrical impulse pattern of premature infants so that they resemble real human brains more than ever.
In the latest study, researchers used this new protocol for functional organoids of the brain using induced pluripotent stem cells (iPSCs) obtained from patients with Rett syndrome. In short, they collected a sample of skin, treated the cells to turn them into iPSCs, and then persuaded them to become brain cells, while preserving each patient’s unique genetic background. To check their results, the team also developed brain organoids that artificially lack this MECP2 Gene and even mixed mutant and control cells to mimic the mosaic pattern typically seen in female patients.
Lack of MECP2 The gene changed many things about the organoids: shape, existing neuron subtypes, gene expression patterns, neurotransmitter production, and synapse formation. Calcium activity and electrical impulses were also decreased. These changes resulted in serious defects in the creation of cortical neuronal oscillation waves, also known as “brain waves”.
In an attempt to make up for the missing MECP2 Gen, the team treated the brain organoids with 14 drug candidates that are known to affect various brain cell functions. Almost all molecular and cellular symptoms were resolved when researchers treated the brain organoids of Rett syndrome with two of the best drug candidates, Nefiracetam and PHA 543613. For example, the number of active neurons in organoids in Rett syndrome roughly doubled after treatment. Nefiracetam and PHA 543613 were previously tested in Phase I and II clinical trials for the treatment of other conditions, meaning they are already known to cross the blood-brain barrier and are safe for human consumption.
According to Muotri, these laboratory-based results provide a convincing argument for the further development of nefiracetam and PHA 543613 in clinical studies for patients with MECP2-deficient neurodevelopmental disorders.
But in the end, the best treatment for Rett syndrome may not be a “super” drug, he said.
“There is a tendency in the neuroscience field to look for highly specific drugs that achieve precise goals and use a single drug for a complex disease,” said Muotri, who is also director of the UC San Diego Stem Cell Program and a member of the Sanford Consortium for Regenerative Medicine. “However, we do not do this for many other complex diseases where multi-pronged treatments are used. Likewise, no goal has fixed all of the problems here. We need to start thinking about drug cocktails that have been successful in treating HIV and cancer. ”
Reference: December 8, 2020, EMBO Molecular Medicine.
DOI: 10.15252 / emmm.202012523
Co-authors of the study are: Cleber A. Trujillo, Jason W. Adams, Leon Tejwani, Allan Acab, Charles A. Thomas, UC San Diego; Priscilla D. Negraes, Cassiano Carromeu, UC San Diego, and StemoniX, Inc .; Ben Tsuda, Terrence J. Sejnowski, UC San Diego and Salk Institute for Biological Studies; Neha Sodhi, Katherine M. Fichter, Fabian Zanella, StemoniX, Inc .; Henning Ulrich, Universidade de São Paulo.
Disclosure: Alysson R. Muotri is a co-founder and an investor in TISMOO, a company dedicated to the genetic analysis and modeling of brain organoids, focusing on therapeutic applications tailored to autism spectrum disorders and other neurological disorders of genetic origin . The terms of this agreement have been reviewed and approved by the University of California at San Diego in accordance with a conflict of interest policy.