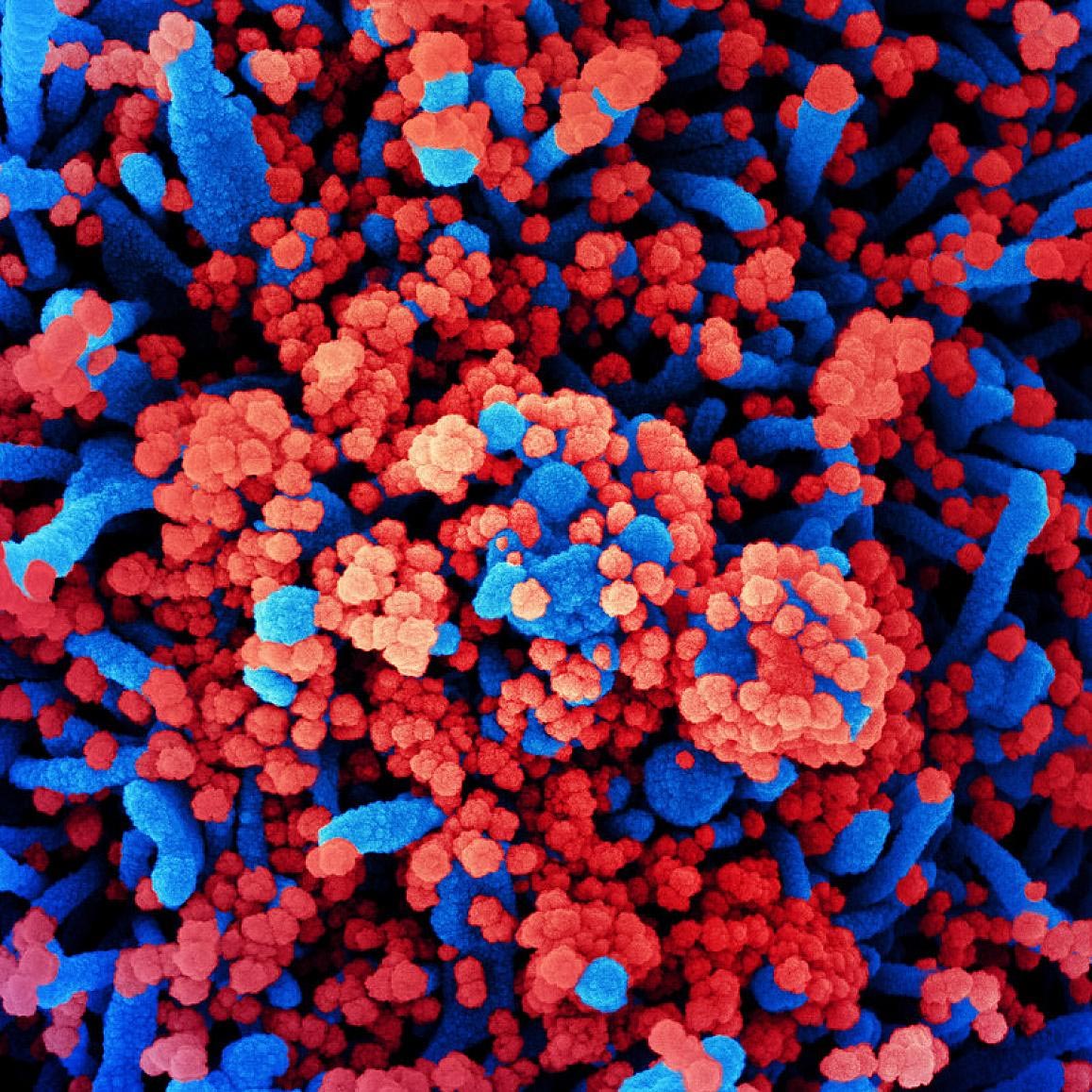
Colored scanning electron micrograph of a cell (blue) that is heavily infected with SARS-CoV-2 virus particles (red) and that was isolated from a patient sample. Image taken at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Image Credit: NIAID
A clinical study by the National Institutes of Health to evaluate the safety and effectiveness of Hydroxychloroquine for the treatment of adults with coronavirus disease 2019 (COVID-19) has officially concluded that the drug has no clinical benefit for hospital patients. Although it was found to cause no harm, early results in June when the study was canceled showed that the drug did not improve outcomes in COVID-19 patients. The final data and analysis of the study, funded by the National Institute of Heart, Lung and Blood (NHLBI), part of the NIH, was published online on November 9, 2020 Journal of the American Medical Association.
The study, titled Findings Related to COVID-19, which was treated with hydroxychloroquine in inpatients with symptomatic disease (ORCHID), began after laboratory studies and preliminary reports that found hydroxychloroquine – which is commonly used to treat malaria and rheumatic diseases such as arthritis will – could show promise in treatment SARS-CoV-2, the virus that causes COVID-19.
The NHLBI’s Network for Clinical Trials Prevention and Early Treatment of Acute Lung Injury (PETAL) started the trial in April in 34 hospitals in the US and included 479 of the expected 510 patients. By June, preliminary evidence showed that hydroxychloroquine was unlikely to be of any benefit.
NIH officials said the careful design, conduct, and monitoring of the study were key to its results, as well as recommending a data and security monitoring committee (DSMB) to stop the study early.
“A rigorously designed clinical trial that captured patient-centered, clinically meaningful results was critical to reaching the firm conclusions about the use of hydroxychloroquine in COVID-19. ORCHID shows hydroxychloroquine does not improve clinical outcomes in hospitalized COVID-19 patients, “said James P. Kiley, Ph.D., director of the division of lung diseases at the NHLBI. “We hope this clear finding will help practitioners make informed treatment decisions, and researchers will continue their efforts to pursue other possible safe and effective treatments for patients with this disease.”
The ORCHID study enrolled participants between April 2 and June 19, who had an average age of 57 years. These included 290 Spanish and black participants and 212 female participants. All participants received clinical care as indicated for their condition. Participants were randomly assigned to a treatment group and received 10 doses of either hydroxychloroquine or placebo over five days. Researchers then assessed the clinical status of each patient 14 days after they were assigned to a treatment group. They used a seven-category scale from one (death) to seven (discharged from hospital and able to do normal activities). The researchers also measured 12 additional outcomes, including death that occurred 28 days after participants were assigned to a treatment group.
On day 14, those who received hydroxychloroquine and those who received a placebo had similar health conditions, with most participants in both groups being discharged from the hospital and being able to do a range of activities. The number of participants in both treatment groups who died on day 14 was also similar. On day 28, 25 of 241 patients in the hydroxychloroquine group and 25 of 236 patients in the placebo group had died.
“The finding that hydroxychloroquine is not effective for the treatment of COVID-19 was consistent across all patient subgroups and across all outcomes evaluated, including clinical status, mortality, organ failure, length of oxygen depletion and length of hospital stay,” said Wesley Self, MD, MPH , Emergency Physician at Vanderbilt University Medical Center and investigator for the PETAL Clinical Trials Network who led the ORCHID trial. He also noted that the finding was consistent with similar studies in the UK and Brazil.
“Our diverse teams of clinicians and researchers have worked quickly in extremely difficult circumstances to achieve what the NIH and the PETAL Network do best: gold standard studies of key issues for patients with life-threatening diseases,” said Samuel M. Brown, MD , MS, an intensive care physician at Intermountain Healthcare and investigator for the PETAL network who led the study. “While we were hoping hydroxychloroquine would help, this too is an important finding as we work together to find effective treatments for COVID-19.”
As of November 9, 2020, the Centers for Disease Control and Prevention has reported more than 9.9 million cases of COVID-19 and more than 230,000 deaths in the United States. Many other randomized clinical trials are currently evaluating the efficacy and safety of other drugs compared to a placebo in the urgent race for effective therapies to treat COVID-19.
Reference: “Effect of Hydroxychloroquine on Clinical Status at 14 Days in Hospitalized Patients in COVID-19A Randomized Clinical Trial” by Wesley H. Self, MD, MPH; Matthew W. Semler, MD; Lindsay M. Leither, DO; Jonathan D. Casey, MD, MSc; Derek C. Angus, MD, MPH; Roy G. Brower, MD; Steven Y. Chang, MD, PhD; Sean P. Collins, MD; John C. Eppensteiner, MD; Michael R. Filbin, MD; D. Clark Files, MD; Kevin W. Gibbs, MD; Stollen A. Ginde, MD, MPH; Michelle N. Gong, MD, MS; Frank E. Harrell Jr., PhD; Douglas L. Hayden, PhD; Catherine L. Hough, MD, MSc; Nicholas J. Johnson, MD; Akram Khan, MD; Christopher J. Lindsell, PhD; Michael A. Matthay, MD; Marc Moss, MD; Pauline K. Park, MD; Todd W. Rice, MD; Bryce RH Robinson, MD, MS; David A. Schoenfeld, PhD; Nathan I. Shapiro, MD, MPH; Jay S. Steingrub, MD; Christine A. Ulysse, MS; Alexandra Weissman, MD, MPH; Donald M. Yealy, MD; B. Taylor Thompson, MD; Samuel M. Brown, MD, MS; for the PETAL Clinical Trials Network of the National Institute for Heart, Lung and Blood, November 9, 2020, Journal of the American Medical Association.
DOI:
The ORCHID study was funded by NIH / NHLBI grants. In addition, the research was supported by the National Center for the Advancement of Translational Sciences with the awards UL1TR001102 and UL1TR002541.